Intracytoplasmic sperm injection, or ICSI, is an in vitro fertilization (IVF) process in which the sperm is introduced directly into the egg to facilitate fertilization and give rise to the new being. Unlike classic IVF, ICSI allows reproductive success in situations of severe male infertility.
In the following article we will talk about the steps that are followed to carry out this process, as well as the indications and probability of pregnancy.
Provided below is an index with the 7 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 2.3.
- 2.4.
- 2.5.
- 2.6.
- 2.7.
- 2.8.
- 2.9.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 6.
- 7.
Indications
The most common situations that require ICSI are:
- Poor quality eggs or with a thickened zona pellucida.
- Valuable semen samples such as frozen samples, samples from cancer patients or samples obtained by testicular biopsy, epididymis or testicle aspiration.
- Poor semen quality, especially in terms of mobility, morphology and concentration. The most frequent seminal alterations are azoospermia, oligospermia, asthenospermia and teratospermia.
- Repeated failure in several classic IVF cycles.
- Necessity to perform the PGD technique (preimplantation genetic diagnosis)
- Men with an infectious disease or infertility of immunological cause.
- Cases in which few eggs are retrieved in the follicular puncture.
Although these are the indications for which ICSI is recommended, there are many assisted reproduction clinics that apply it to any type of fertility problem that requires in vitro fertilization, that is, they do not use the conventional method although it is possible.
FIV-ICSI step by step
In vitro fertilization through sperm microinjection follows the same steps as conventional IVF except at the time of the union of egg and sperm. The main steps are:
Ovarian stimulation
In order to obtain a greater number of eggs, the patient receives ovarian stimulation treatment through subcutaneous administration of hormonal medication.
These injections promote the development and maturation of a large number of eggs in the same cycle, which increases the likelihood of obtaining viable embryos and thus the likelihood of pregnancy.
During the treatment, the patient will have to go to the clinic to undergo the analytical and ultrasound controls necessary for the process to go well.
This treatment lasts between 7 and 12 days approximately. In the first phase, drugs are given to stimulate ovarian production (GnRH analogues and gonadotropins) and, in the second phase, 36 hours before follicular puncture, the hCG hormone is given for final maturation and ovulation induction.
If you want to know more about this assisted reproduction method, we recommend you read the following article: Ovarian stimulation.
Follicular puncture
Also known as ovarian puncture. This is the surgical intervention in which the eggs are obtained by aspiration of the liquid from the follicles (structures of the ovary where the eggs mature).
This is a simple operation of between 15 and 30 minutes that is performed under sedation or mild anesthesia. It does not require hospitalization or prolonged rest.
Once in the laboratory, the follicular liquid is analyzed in search of the eggs, which will be later decumulated, that is to say, the layer of cells of the cumulus-crown that surrounds them will be eliminated.
More information about this process here: What is ovarian punction?
Semen collection
Sperm sample is usually obtained by masturbation after a period of abstinence of 3 to 7 days. If it is not possible to obtain semen by ejaculation, it will be obtained directly from the testicle through biopsy or aspiration.
In order to realize ICSI, the semen previously passes through the puported sperm capacitation. This is a process that allows the sample to be concentrated into good quality spermatozoa, eliminating seminal plasma and immobile or dead spermatozoa.
There are some valuable sperm samples that are used directly, without being capacitated.
Decumulation
Decumulation is the process in which the eggs obtained in follicular puncture are deprived of the layer of cells that surrounds them: the cells of the crown-cumulus complex.
To facilitate microinjection, these cells are removed both mechanically (by passing the egg through decreasing calibre pipettes) and chemically through specific solutions.
This step is not performed in conventional in vitro fertilization.
Insemination or fertilization
It is the moment in which egg and sperm fuse to create the new being. It is done in the microinjector.
The specialist holds the egg with one of the microinjector's needles, the purported holding needle, the ends of which are blunt. With the other needle, with its sharp end, he aspirates a spermatozoon and inserts it completely into the ovum, waiting for both nuclei to fuse and give rise to the zygote (embryo of a cell).
Analyzing fertilization
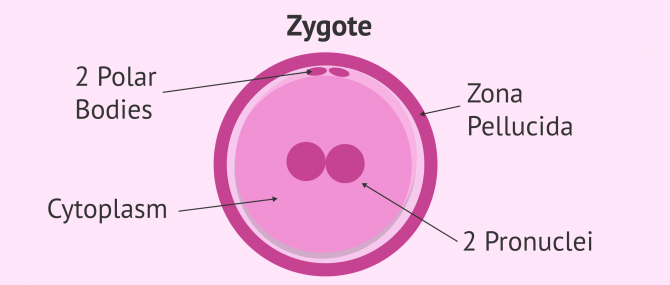
After microinjection, the eggs are left in the incubator and about 16-20 hours later it is checked whether they have been correctly fertilised, i.e. if they have given rise to zygotes, or if, on the contrary, there has been fertilization failure.
It is said that fertilization has occured when we distinguish 2 polar corpuscles (CP) and 2 pronuclei (PN), the feminine and the masculine, which will fuse later to begin embryonic development.
Embryo culture
Fertilised eggs, i.e. embryos, will be left in culture until the day on which they are to be transferred or frozen. They will be left in special incubators that maintain the conditions of pressure, light, gas concentration and optimum temperature for their growth.
Throughout the cultivation period, the different embryonic qualities will be evaluated in order to assess their quality. Some of the factors analyzed are: division rhythm, cell size, fragmentation, number of cells...
In this link you’ll get more information: What are the parameters for embryonic quality?
The embryos will remain in culture for a period of 3 to 6 days, depending on whether they are to be transferred in embryonic stage (day 3) or in blastocyst stage (day 5-6). Good quality embryos that had not been transferred will be cryopreserved for future treatments.
Endometrial preparation and transfer
The patient will receive hormonal medication treatment based on estrogen and/or progesterone orally or vaginally. The objective of these medication is to ensure that the endometrium acquires the appropriate appearance and thickness so that the embryos can be implanted and thus achieve gestation.
When the doctor determines through ultrasound that the endometrium is ready, the embryo transfer will be done. This is a painless process of about 10 minutes in which the embryos are deposited in the uterus of the woman waiting to implant and start the pregnancy.
The number of embryos to be transferred should be chosen by the woman or couple, always considering the advice of the specialist for each personal situation. Only embryos of highest quality will be transferred.
Embryo vitrification
Viable embryos that have not been transferred will be cryopreserved by the embryo vitrification process. It is an ultra-fast freezing technique that allows the embryos to be kept indefinitely without practically altering their qualities.
The embryo survival rate is above 90%, so they may be used for other treatments in the future.
Differences between conventional IVF and ICSI
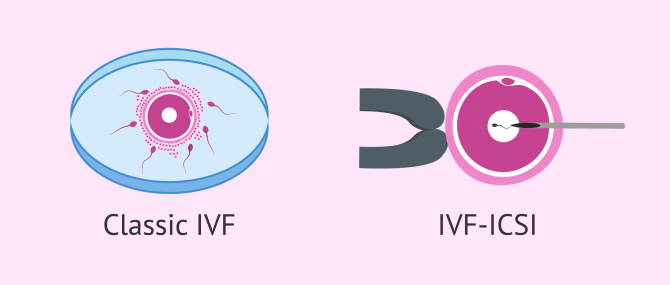
Until the moment of fertilization, the procedure between both techniques is the same: ovarian stimulation, puncture for the extraction of oocytes and semen collection.
In classic IVF, the egg (not decumulated) comes into contact with a drop of semen in which there are thousands of sperm, of which only one will be able, by his own means, to introduce the head into the egg to give rise to the embryo. In other words, fertilization itself is carried out by the same spermatozoon without human help.
In ICSI, on the other hand, it is the embryologist who, thanks to microinjection, introduces the previously selected sperm directly into the ovum. In addition, the egg has undergone a decumulation process, a step that is not carried out in traditional IVF.
Due to the greater complexity of the technique and the need for specific instrumentation such as the micromanipulator, the ICSI technique makes the in vitro fertilization procedure more expensive. In addition, it requires a special skill on the part of the embryologist who is going to perform the microinjection.
Read more about the differences here: IVF or ICSI?
ICSI and surrogacy
Surrogacy is usually performed through an in vitro fertilization process, either conventional or ICSI.
ICSI will be done if PGD is going to be applied, something common in surrogacy processes, or if the gametes require it.
The process is exactly the same as we have mentioned, with the only difference that the endometrial preparation and transfer will take place in the uterus of the gestational carrier ("surrogate mother") and not of the future mother.
As for the rest of the steps, it will depend on the origin of the eggs. If the eggs of the future mother are to be used, she will undergo ovarian stimulation and follicular puncture. If, on the other hand, egg donation is used, it will be the donor who undergoes the first part of the process.
You can get more information here: What is surrogacy?
FAQs from users
What are the main risks of ICSI?
The main problems or consequences that may result from ICSI are due to ovarian stimulation. This treatment, if not properly regulated, can lead to the so-called Ovarian Hyperstimulation Syndrome .
Another problem is multiple pregnancy, the probability of which increases if the transfer is of more than one embryo. The twin pregnancy is more risky than the single pregnancy, so it is recommended to choose the number of embryos to choose responsibly and always considering the advice of the specialist.
Finally, the risk of miscarriage and ectopic pregnancy is also slightly higher when applying ICSI compared to natural conception.
If you want more information about those risks, click here: .
Which method will produce better results: ICSI or classiv IVF?
It will depend on each situation. For example, if we are dealing with a case of severe male infertility, conventional IVF will probably not allow viable embryos to be obtained. Therefore, in this case, ICSI will offer a better chance of success.
However, in normal situations of good quality of both gametes, both techniques will offer good results.
Is hatching recommended in an IVF-ICSI cycle?
In order for the embryo to implant in the uterine endometrium, it must break and leave the covering (zona pellucida) that surrounds it. The hatching is what is known as the rupture of this membrane to allow the exit of embryonic cells and implantation.
Therefore, assisted hatching is nothing more than making a small hole in the zona pellucida of the fertilized egg, or embryo, to facilitate implantation.
In some IVF-ICSI situations, it is convenient to make hatching to facilitate implantation. One situation in which it would be beneficial to make this small hole is in those embryos with a thickened zona pellucida.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Reproduccion Asistida ORG, 2018, Microinyección espermática: ¿Qué es la ICSI y cuál es su precio? Aitziber Domingo, Miguel Dolz, Rebeca Reus y Susana Cortés Gallego, https://www.reproduccionasistida.org/microinyeccion-intracitoplasmica-de-espermatozoides-icsi/
Reproduccion Asistida ORG, 2019, La reproducción asistida: tipos, precio y Seguridad Social. Blanca Paraíso, Miguel Dolz, Sara Salgado y Zaira Salvador, https://www.reproduccionasistida.org/reproduccion-asistida/
FAQs from users: 'What are the main risks of ICSI?', 'Which method will produce better results: ICSI or classiv IVF?' and 'Is hatching recommended in an IVF-ICSI cycle?'.
Author