In the process of surrogacy, the surrogate must pass a psychological evaluation in addition to undergoing a series of medical and genetic tests for pregnant women. After a positive pregnancy test, she has to follow a rigorous medical check-up schedule.
The goal is both to prevent health problems and to prevent fetal and perinatal problems in the future baby. The intentional parents are the ones who bear all the medical costs of pregnancy.
Provided below is an index with the 5 points we are going to expand on in this article.
- 1.
- 2.
- 2.1.
- 2.2.
- 3.
- 4.
- 4.1.
- 4.2.
- 4.3.
- 4.4.
- 4.5.
- 4.6.
- 5.
Before Pregnancy
It is important to know why a woman offers to gestate other people's babies. To select a pregnant woman, determinants of her health are taken into account:
- Lifestyle
- Gynaecological medical history
- Family history
- Mental and emotional balance
One of the conditions so that gestation does not pose a risk to either the pregnant woman or the future baby is that she is in an optimum state of health at the time of the embryo transfer.
For this purpose, a rigorous physical and psychological examination will normally be carried out in order to rule out serious illnesses or associated problems that could affect the pregnancy.
In surrogacy, in vitro fertilization (IVF) treatment involves not using the oocytes of the surrogate, but of the mother of intention or of an oocyte donor. It will be necessary to wait from 13 to 14 days after the pregnant woman has started treatment with progesterone to perform the first medical tests.
They should not be done too early because, before this deadline, embryonic activity still does not produce enough hCG hormone to confirm pregnancy and could result in a false negative.
The hCG blood test performed in the laboratory is more reliable than the urine test as it is able to detect smaller concentrations, from 10 mUI/ml. The first ultrasound is usually done at the end of the first trimester, in week 12.
During pregnancy.
In the first consultation, once it is known that the transfer has been positive and therefore there is pregnancy, the gynecologist controls the weight, heart and blood pressure. In addition, a gynecological examination and ultrasound are performed to determine the appearance and heartbeat of the embryo. This is usually done between the second and third week after the transfer.
In this visit is when they usually give the guidelines to follow during pregnancy: food, exercise, hygiene, sexual relations, etc..
From then on, the pregnant woman's medical check-up follows a month-to-month calendar of essential medical tests to detect any anomaly in time. The usual frequency of ultrasounds or ultrasound monitoring is one for each trimester of pregnancy, specifically at weeks 12, 20 and 36, but additional ultrasounds may be requested as needed.
The second visit is usually made at the beginning of the second trimester between 11 and 13 weeks of pregnancy. The size of the baby is assessed by ultrasound, the nuchal fold is measured and possible malformations are ruled out. It is also common to perform a prenatal diagnostic blood test.
Between 16 and 17 weeks, the usual analyses will be carried out for each visit:
- Study of swelling of hands and feet
- Belly measurement
- Weight control
- Blood pressure
- Baby Heartbeat
- Ultrasound
- Palpation of the abdomen to determine fetal position and movement
At the fifth month, the baby is measured and his or her organs and limbs are examined closely to rule out possible malformations.
In the sixth month of pregnancy, the second routine test is performed, which includes a sugar test to rule out gestational diabetes.
Invasive and non-invasive genetic testing
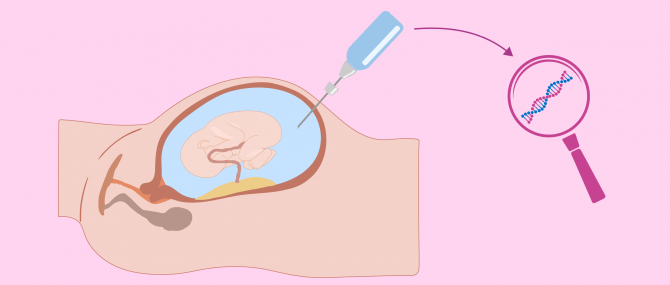
From the first weeks of pregnancy a series of genetic tests can be carried out that will allow malformations and anomalies to be detected. These tests will be invasive or non-invasive depending on whether or not they require physical penetration into the body.
Amniocentesis and chorionic biopsy (also called chorionic villus samples or CVS) can diagnose chromosomal abnormalities and birth defects. They let us know, for example, if the baby has Down syndrome.
- Amniocentesis -removal of a sample of amniotic fluid for analysis between 16 and 20 weeks
- Chorionic biopsy -removal of a piece of chorion (the outer sheath covering the embryo). It is performed between weeks 10 and 12
In contrast, triple screening is a combination of non-invasive tests that can be performed in the first trimester. It is based on the biochemical analysis of hormones present in the blood of the surrogate. It allows to evaluate the risk of malformations or certain genetic anomalies among which we find Down syndrome. It is not a diagnosis but indicates a low, moderate or high risk.
Non-invasive prenatal genetic testing can be done as early as the 10th week of pregnancy. It analyzes the DNA of the fetus present in the blood of the pregnant woman.
Twin Pregnancy Tests
IVF increases the risk of multiple pregnancy when, to improve the chances of success, more than one embryo is transferred into the uterus. Although many intentional parents do not see it as a problem, at the medical level twin pregnancies can lead to a number of complications.
Both amniocentesis and chorionic biopsy are invasive tests that become more delicate when the pregnant woman expects more than one child. Samples should be taken from each baby without confusing them. In the case of triplets or more babies, you don't always get them.
In addition, the risk associated with these tests increases in the case of a multiple pregnancy. The rate of miscarriage is multiplied by five after amniocentesis and by four after chorionic biopsy.
Thanks to the Preimplantation Genetic Diagnosis (PGD) procedure, it is possible to extract one or more cells from the embryos in order to analyse their genetic material. In this way, chromosomal alterations can be ruled out and the chances of transferring a suitable embryo can be increased. For this reason it is increasingly advisable to transfer a single embryo to avoid twin pregnancy without reducing the chances of success.
At the end of pregnancy
If so far everything is correct and the pregnancy is going well, the next visit will be between the 35th and 38th weeks of pregnancy. A vaginal and rectal culture is done here to rule out streptococcus agalactiae, which can cause an infection in the baby. In case of a positive result, an antibiotic will be prescribed to the pregnant woman.
If the placenta is low, an ultrasound is done to check that there is no obstruction of the cervix. The baby's position is reassessed.
Childbirth usually occurs at 40 weeks' gestation; however, some pregnancies last longer. In these cases, the baby's heartbeat and uterine contractions are studied at 40 and 41 weeks of pregnancy. The baby's movements and muscle tone, as well as the amount of amniotic fluid, are sometimes monitored. At 42 weeks, labour is induced if it has not been triggered on its own.
During the third trimester, the weight of the fetus is already a greater burden. The body changes and the center of gravity changes. However, the pregnant woman may maintain a minimum physical activity until the last month.
Performing postural control exercises and breathing exercises will allow you to prepare your body for labor and postpartum recovery. Walking daily will help the pregnant woman feel better, as well as practicing specially adapted activities such as yoga exercises for pregnant women.
FAQs from users
What psychological tests should be done on the surrogate pregnant woman to ensure that she is prepared for it?
First of all, any psychological pathology should be ruled out. There are quite reliable tools to determine the state of emotional health. In addition, an in-depth interview should be carried out to determine the motivation, maturity and freedom of judgement of the pregnant potential.
Can a woman with HIV be surrogate?
In the process of surrogacy, a woman with HIV will be discarded because she does not have optimal health conditions. An HIV-positive woman can transmit HIV to the baby at any time during pregnancy, with increased risk during childbirth.
If a woman chooses to become pregnant despite having HIV, she will receive medication during childbirth to reduce the risk of mother-to-child transmission and a cesarean delivery will be preferred.
Are any special tests done on the pregnant woman at the end of the pregnancy?
At week 33 or 34 the last blood tests are done to measure the levels of hemoglobin, red blood cells and iron. Blood coagulation levels are checked and hepatitis B and C, toxoplasmosis, HIV and sexually transmitted diseases are repeated.
Vaginal culture between 35 and 38 weeks of pregnancy detects Streptococcus agalactiae (strep) bacteria. If it is positive, the pregnant woman receives antibiotics.
As the date of birth approaches, periodic fetal monitoring is done to record the baby's heartbeat and to detect the pregnant woman's contractions.
How can it affect the baby if the surrogate gets toxoplasmosis?
Toxoplasmosis is a mild parasitic infection in healthy adults, but during pregnancy, the parasite can infect the placenta or fetus. The baby born with congenital toxoplasmosis can suffer structural and neurological problems. In the most severe cases, it may be born lifeless.
Is it necessary for the pregnant woman to carry out all the genetic tests?
During IVF, PGD (preimplantation genetic diagnosis) is recommended to rule out embryos with chromosomal alterations.
During pregnancy, invasive tests such as amniocentesis and chorionic biopsy allow reliable diagnoses, but always involve a small risk. Therefore, genetic testing is not mandatory in low-risk pregnant women.
The selection criteria of the pregnant woman (age, state of health, habits, previous gestation experience...) serve to rule out the greatest number of risk factors.
The gynaecologist will determine which tests are necessary in each case.
What are the general requirements for a woman to become a surrogate?
The requirements depend on each country. For example, in the case of the USA, the woman who wants to be part of this process must undergo medical and psychological check-ups.
Normally, they are women who have already formed a family, who have their own children and want to help other people. In addition, they must have an interview with the intended parents to get to know them.
This is because, in the USA, the pregnant woman chooses the couple whose child she wants to gestate and the future parents or intentional parents choose the surrogate. We must keep in mind that this is an agreement between two parties.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
FAQs from users: 'What psychological tests should be done on the surrogate pregnant woman to ensure that she is prepared for it?', 'Can a woman with HIV be surrogate?', 'Are any special tests done on the pregnant woman at the end of the pregnancy?', 'How can it affect the baby if the surrogate gets toxoplasmosis?', 'Is it necessary for the pregnant woman to carry out all the genetic tests?' and 'What are the general requirements for a woman to become a surrogate?'.