Pre-implantation genetic diagnosis or PGD is a technique for analyzing embryos to differentiate those that are carriers of a genetic abnormality from those that are genetically normal.
The final objective of this technique is to avoid the birth of children with chromosomal abnormalities since embryos diagnosed as abnormal are discarded for transfer. This increases the probability of embryo implantation and therefore the probability of successful in vitro fertilization (IVF) treatment.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 3.1.
- 4.
- 4.1.
- 4.2.
- 5.
- 5.1.
- 5.2.
- 6.
- 7.
- 7.1.
- 7.2.
- 7.3.
- 7.4.
- 8.
- 9.
Definition of PGD
PGD stands for preimplantation genetic diagnosis. This is a technique that makes it possible to eliminate the probability of transmission of genetic diseases from parents to children. PGD normally detects point mutations in embryos that cause serious genetic diseases.
Thanks to PGD, it is possible to select those normal embryos from a group in which the proportion of abnormal embryos with genetic alterations is suspected to be above normal. Therefore, it is extremely important to perform PGD in an IVF cycle before transferring the embryos into the mother's uterus.
The main reason for performing PGD is that the morphological selection of the embryos does not allow the discarding of embryos with chromosomal abnormalities, so an embryo can be classified as being of good quality and genetically abnormal.
It should be noted that PGD is not the same as a prenatal diagnosis since the latter is useful for detecting abnormalities during pregnancy.
When is PGD applied?
Primarily, PGD technology is indicated as a complement to the IVF-ICSI process in the following situations:
- When one or both partners (those who provide the eggs and sperm) are carriers of a disease or genetic abnormality.
- When one or both members of the couple have an altered karyotype, that is, an alteration in the number of chromosomes.
- Repeated implantation failure.
- Repeated miscarriages.
- Advanced maternal age. The probability of genetic abnormalities in the embryo increases proportionally with the age of the mother. Thus, after the age of 35, the proportion of morphologically normal embryos with aneuploidies, i.e. genetic abnormalities, increases. This percentage is even higher in women over 40.
- Family history of disease or genetic alteration.
It is necessary to know that the genetic diagnosis of the embryos implies the manipulation of these, which can be a risk. For this reason, it is important to assess the risk-benefit balance and perform the procedure only when it is necessary and can improve the chances of success.
Steps in the genetic analysis of embryos
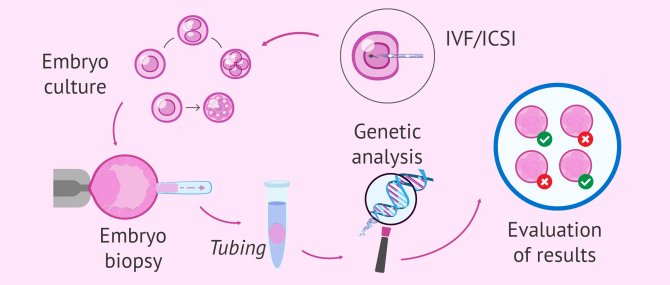
PGD is a complementary technique to the IVF process (in vitro fertilization) Below are the steps to follow in order to perform PGD on the embryos before their transfer to the uterus:
- Egg fertilization: is performed using the ICSI technique (intracytoplasmic sperm injection) and not conventional IVF. This avoids the possible interference of the sperm that remain attached to the egg membrane in conventional IVF.
- Embryo culture: The embryos are left in culture until day 3, at which time they have between 6 and 8 cells. It is also possible to extend the culture until day 5-6 when the embryo is in the blastocyst stage, formed by two cell groups: the inner cell mass (which will give rise to the embryo) and the trophoectoderm (which will form the placenta).
- Embryo biopsy: With the use of a laser or chemical components a small hole is made in the zona pellucida and one or two cells are extracted through it (embryos on day 3) or a small set of cells from the trophoectoderm (blastocyst on day 5). It is important to see that the tested cells have a single nucleus (where the DNA is stored) to avoid altering the results.
- Tubing: consists of depositing, with special delicacy, the cells obtained from the embryo in a tube specialized for this process.
- Genetic analysis: the cells in the tube are analyzed using molecular biology techniques such as PCR, FISH, CGH array or NGS.
The results obtained will indicate whether the embryo analyzed has a normal chromosomal endowment or if, on the contrary, it presents a genetic alteration that could lead to disease.
Considerations of the PGD process
It needs to be remembered that, at this point, the embryo is at a very early stage of development and its cells are totipotent stem cells, i.e. they can differentiate into any type of cell in the human body until they form a complete organism. For this reason, the extraction of one or two cells from the embryo will not affect its further development.
Nor should it be forgotten that through this technique the genetic endowment of one or a few cells of the embryo is analyzed. Therefore, the reliability of the result, although close, is not 100%. One possibility is the development of what is known as mosaicism, a phenomenon in which some cells have different genetic information from others.
Pros & Cons
As we have highlighted before, the genetic analysis of embryos allows us to avoid the transfer of embryos with genetic abnormalities that could lead to children with serious diseases.
There are genetic alterations incompatible with life that, in the event of a transfer, would result in implantation failure or abortion. However, there are other abnormalities that can lead to the birth of children with developmental disorders. An example of the latter case is found in chromosomal syndromes such as Down syndrome (trisomy 21), Patau syndrome (trisomy 13), Edwards syndrome (trisomy 18), etc.
Advantages of PGD
When people decide to do PGD when trying for pregnancy, they can achieve the following benefits:
- Avoid the transfer of aneuploid embryos, that is, with chromosomal alterations before their transfer. It therefore allows for the transfer of healthy embryos.
- Increases the rate of implantation.
- Increased pregnancy rate.
- Reduced abortion rate.
- Decreases the risk of children born with chromosomal syndromes known as Huntingon's disease and muscular dystrophy, for example.
Disadvantages of PGD
Like any assisted reproduction technique, on the other side of the coin, we find the negative consequences of performing PGD. We’ll show some of them below:
- It involves embryo manipulation. During the biopsy, the embryo is outside the incubator and this can alter its qualities. On many occasions, there are embryos that are unable to withstand the process and end up stopping their development, despite being genetically normal.
- Need to cancel the transfer because none of the embryos obtained are healthy. It should be kept in mind that there are genetic alterations with mild symptoms or that are not very life-threatening. However, the legislation does not allow the transfer of embryos detected with genetic abnormalities through PGD.
- Doing PGD does not make the need for prenatal testing redundant in the most serious cases (family history of genetic disease, parents with some abnormality, etc).
- Ethic issues. Especially those who believe that life begins from the very moment fertilization occurs, consider that discarding embryos for transfer is to prevent their life.
New techniques of embryo manipulation and advances in reproductive medicine are making the effect on embryos less and less harmful. Yet it is still a risk.
What does the law say about PGD?
United Kingdom and United States of America do not have the same vision about PGD process use.
United Kingdom
European Commission's science and knowledge service in its report about Preimplantation Genetic Diagnosis in Europe says that:
The Since PGD involves creation, storage and use of embryos outside the body, it requires a licence from the Human Fertilisation and Embryology Authority (HFEA), the UK regulatory body for this area.
The HFEA receives its authority from the Human Fertilisation and Embryology Act of 1990 and Human Fertilisation and Embryology Bill of 2007.
PGD is authorized under the following situations:
- Detection of serious hereditary diseases, of early onset and without postnatal curative treatment.
- Detection of alterations that may compromise embryo viability.
Indeed, it can be used to select against severe medical conditions or to select a human leukocyte antigen (HLA) match for a sick relative.
United States
On the contrary, in the USA, there are no federal or state laws that regulate the use of PGD. So, the use of PGD is left to doctors' discretion.
According to the Comparative preimplantation genetic diagnosis policy in Europe and the USA and its implications for reproductive tourism present on the website of US National Library of Medicine and National Institutes of Health:
The genetic testing process itself (i.e. the analytic quality of the tests and the qualifications of the technicians who carry them out) are subject to the Clinical Laboratory Improvement Amendments (CLIA).
Thus, in the United States, PGD can be performed for example in order to select the gender of the future baby, that is why this technique is seen as controversial.
PGD and surrogacy
The surrogacy process is usually performed by in vitro fertilization. For this reason, it is possible to carry out the analysis of the embryo's genes through PGD.
In fact, it is something that is usually done, especially in the United States, the preferred destination for surrogacy treatment. However, it is important for intended parents to know both the benefits and disadvantages of PGD when not responding to specific indications.
While it is true that we reduce the likelihood of miscarriage, as well as possible ethical complications, it may be that, as we have already said, the embryos are not capable of surviving the process and we cannot perform the transfer because viable embryos are not available.
FAQs from users
When is PGD recommended?
PGD is recommended to identify embryos that are at risk for a single gene disorder, e.g. cystic fibroses, and for testing for chromosomal structural rearrangements, e.g. translocations, deletions/duplications. PGS or now called PGT, preimplantation genetic testing, is used to detect aneuploidy.
Can PGD be done on frozen embryos?
Yes, it is possible to freeze the embryos, thaw them and then do a biopsy to analyze them genetically. In any case, this is not usual. Generally, what is done is to leave the embryos in culture until the day of the biopsy, either on day 3 or day 5.
The protocol to follow will depend on each laboratory and the personal situation of the patients.
How much does pre-implantation genetic diagnosis cost?
Performing PGD on embryos implies an increase in the cost of in vitro fertilization of between 3,000 and 4,000 euros approximately. Therefore, the total price of an IVF-DGP process is around 9,000 euros.
Would preimplantation genetic diagnosis help prevent the inheritance of cystic fibrosis?
Yes, cystic fibrosis is one of the diseases susceptible to genetic analysis before implantation.
Suggested for you
As we have mentioned, PGD involves the manipulation of embryos as an Assisted Reproductive Technology. If you want to learn more about the techniques performed in Assisted Reproduction, we recommend you to read the following post: Assisted Reproductive Technology (ART) – Techniques Used in Surrogacy.
Some of the most common diseases for which PGD is requested have also been included in the article. In this article you have more explanation about it: What Genetic Diseases Can PGD Test for?
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
The European Commission's science and knowledge service about Preimplantation Genetic Diagnosis in Europe: [ici]
Comparative preimplantation genetic diagnosis policy in Europe and the USA and its implications for reproductive tourism by US National Library of Medicine and National Institutes of Health [ici]
FAQs from users: 'When is PGD recommended?', 'Can PGD be done on frozen embryos?', 'How much does pre-implantation genetic diagnosis cost?' and 'Would preimplantation genetic diagnosis help prevent the inheritance of cystic fibrosis?'.



It’s actually a fantastic thing that you can prevent severe illness in the future baby. Some might find it controversial and unethical but for me, it’s way more unacceptable to accept the possible risk of having a baby who might develop a severe health condition in the future and whose life quality will enormously be compromised due to the selfishness of the parents.
Hi, my name is Mariana and I’m 42 years old and my husband is 41. I already have two children, from another relationship. My new husband and I have been trying to become parents for years but we have never been able to carry the pregnancy to term and we have never had a clear diagnosis. We think it is embryo implantation failure before when I was not on the treatment I always noticed that taking antibiotics (when I had a throat infection) caused me to delay my period as if I were being pregnant, and after 3-6 days my period was very heavy. I always wondered if I was pregnant and the embryo implanted, but my uterus was not receptive. After inseminations and 4 in vitro failures, we have talked to our doctor and I have mentioned that during the last 4 years in the ultrasounds made are 5 small fibroids that are the cause of the current discomfort I have, for example: urged desire to urinate, feeling of a full bladder. The same OB/GYN who has performed the last 3 invitros (the first invitro was with an egg embryo and the other one of us, the last 4 with blasts of us) sent me to the urologist, everything is fine. The discomfort is due to the fibroids is what I have discovered researching on the Internet, although I do not know if it is another serious thing.
I just went to a clinic for endometriosis and my suspicions were true I have fibroids, and I have been offered 2 alternatives: the first if I no longer want to suffer these problems because they affect my quality of life is to remove my uterus because the doctor says that adenomyosis is fibroids that are difficult to remove. The second is to take a 3-month treatment with Gnr, vitamins, to follow a diet with insulin resistance (with a Nutriologist) and end up doing an IVF. I don’t know what to do. A friend tells me that I better go to a specialist in implantation failure. My doctor says to try a new in vitro but to do the implantation test one cycle earlier. We’re already afraid to try again but we’re looking forward to a baby.
Thank you for your help.
Hi, my husband has brugada syndrome. We have a one year old son who has inherited the genetic mutation for this disease and I would like to know if there is an option if we have another child who does not carry this gene (SCN5).
Hi, I’ve had three embryo transfers that have passed the PGD, and all negative. They always tell me I have a trilateral endometrium, and with perfect measurements, but I still haven’t achieved pregnancy… What could be wrong?
The assumption is that with PGD there’s a better chance of pregnancy, but still..