When a couple has been having unprotected sex for a year and does not achieve a pregnancy, there may be problems with sterility. Therefore, it would be advisable for the couple to see a specialist for the necessary fertility tests.
Specifically, to study a woman's fertility, a series of tests are performed such as transvaginal ultrasound, blood hormone analysis and hysterosalpingography. The set of results obtained will serve the specialist to indicate the state of the patient's fertility and, therefore, to determine which assisted reproduction treatment is the most appropriate to achieve pregnancy.
Besides, there are other complementary tests for the assessment of female fertility, such as hysteroscopy, karyotype and endometrial biopsy.
Provided below is an index with the 9 points we are going to expand on in this article.
- 1.
- 2.
- 3.
- 4.
- 5.
- 5.1.
- 5.2.
- 5.3.
- 6.
- 6.1.
- 6.2.
- 6.3.
- 6.4.
- 7.
- 8.
- 9.
When is a female fertility study performed?
A fertility study is generally recommended when a couple has been seeking pregnancy for a year without success. At this point, the specialist will request various tests from both members of the couple in order to determine the cause of infertility.
Specifically speaking, the main tests for the study of female fertility are the following:
- Vaginal ultrasound to assess the anatomy of the uterus and ovaries.
- Hormone analysis that helps control the menstrual cycle.
- Hysterosalpingography to study the permeability of the fallopian tubes.
- Karyotype to diagnose possible alterations at chromosome level.
If any of these tests show altered results, the doctor will order additional tests, such as an endometrial biopsy and hysteroscopy. Apart from that, the doctor must treat each patient individually when requesting the necessary tests.
Complete gynecological examination
The most important test in gynecological screening is the vaginal ultrasound. Through this non-invasive screening test, the specialist checks the condition of the uterine cavity and the ovaries. In this way, it is possible to see if there is any alteration or anomaly that could make conception difficult.
It is also possible to perform an antral follicle count by means of vaginal ultrasound in order to get an approximate ideo of the woman’s ovarian reserve. A value of 8 or more antral follicles is usually indicative of a good ovarian reserve.
Another test that is often included in gynecological screening is cytology, also known as a Pap smear. This technique involves taking a small sample of cells from the cervix for analysis in the laboratory. Pap smears can detect infections and foreign changes in cells that may indicate the development of cervical cancer.
Female hormone analysis
The menstrual cycle of a woman is regulated by hormones. Any irregularity in hormone levels can affect female fertility. Therefore, performing a hormonal blood analysis helps a great deal when it comes to knowing the fertility state of a woman. In addition, this hormone study also reports on the woman's ovarian reserve and whether the ovaries are functioning properly.
Generally, the blood test is done on day 3 of the ovarian cycle, considering the first day of the cycle when the woman's menstruation sets in. It is also possible that some hormones, such as progesterone, are tested on day 21 of the menstrual cycle.
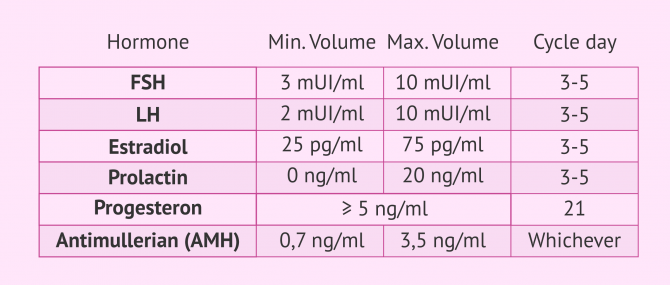
A multitude of hormones can be included in this analysis, but the most relevant to the study of female fertility are:
- FSH (follicle-stimulating hormone)
- is a gonadotropin released by the pituitary gland and responsible for activating ovarian development. Normal FSH values are between 3 and 10 mUI/ml. FSH levels below 6 indicate an excellent ovarian reserve, values of 6 to 9 are good, 9 to 10 moderate and above 10 usually indicate a low ovarian reserve. The determination of this hormone is done between day 3 and 5 of the menstrual cycle.
- LH (luteinizing hormone)
- is also a gonadotropin released by the pituitary gland that exerts its function on the ovary, causing ovulation. The range of value considered normal for the LH hormone is 2 to 10 mIU/ml. The analysis of this hormone is done between day 3 and 5 of the menstrual cycle.
- Estradiol
- hormone released by the ovary as oocyte development progresses. This hormone should have a blood value between 25 and 75 pg/ml. However, ideally on the third day of the cycle the amount of estradiol should be below 50 pg/ml. The analysis of this hormone is done between day 3 and 5 of the menstrual cycle.
- Prolactin
- this hormone is released by the pituitary gland. Its normal level is between 0 and 20 ng/ml on day 3-5 of the menstrual cycle. When prolactin is above normal values it causes what is known as hyperprolactinemia.
- Progesterone
- on the 3rd day of the cycle, this hormone should be below 1.5 ng/ml, as it is released by the corpus luteum and is not generated until ovulation occurs (which is usually in the middle of the cycle). For the value of this hormone to give us information, it must be analyzed on day 21 of the cycle. At this time, you should have a blood level above 5 ng/ml, as this indicates that ovulation has taken place. In any case, ideally it should be above 10 ng/ml.
- Antimullerian Hormone (AMH)
- is a hormone released by the ovarian follicles and is considered a good indicator of ovarian reserve. This hormone can be tested on any day of the cycle, as it is independent of the cycle. An AMH value of between 0.7 and 3.5 ng/ml indicates a good ovarian reserve. The lower the ovarian reserve, the lower the AMH value.
Although these are the basic hormones being studied, it is also possible to analyze others such as thyroid stimulating hormone (TSH), free thyroxine (T4), free triiodothyronine (T3) or testosterone. Although they are not sex hormones, altered levels can negatively affect the hormones that regulate the menstrual cycle and ovulation.
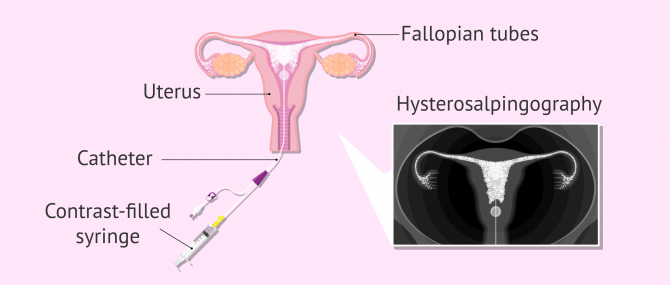
Hysterosalpingography (HSG)
Hysterosalpingography is a diagnostic test that allows us to study the permeability of the fallopian tubes and to observe the structure of the uterus. Since fertilization (union of egg and sperm) takes place inside the fallopian tubes, it is essential to see if passage through them is possible.
The process for hysterosalpingography involves passing a radio-opaque contrast material (liquid that does not allow radiation to pass through and therefore allows visualization when X-rays are applied) through a catheter placed in the woman's reproductive system. If the fluid doesn't find any obstacles in its way, it will exit into the pelvic cavity. Otherwise, if there is a blockage in the fallopian tubes, the fluid could not get through.
The application of X-rays will allow us to visualize the path of the contrast and analyze if there is any blockage in the tubes, as well as any malformation in the uterine cavity.
The result obtained from the hysterosalpingography may be:
- Positive
- indicates that the tubes are permeable and therefore contrast is seen to pass through the two tubes and be expelled into the abdominal cavity.
- Negative
- whether unilateral or bilateral, it means that one or both tubes are blocked and, as a consequence, do not allow contrast to pass through their structure. When this happens, the fallopian tubes inflate. It is also possible that the fallopian tubes may not be visible due to a tubal or uterine malformation.
If the tubal obstruction is mild, this test can help unblock the tube and allow passage through it again. However, this happens in specific cases. In addition, this test is especially important when it comes to establishing the best fertility treatment for each specific case.
Other complementary tests
In some cases, additional procedures to those discussed so far are required. These are resources that are only necessary to deepen the study of female infertility.
Other relevant tests performed on women for the study of sterility are detailed below.
Caryotype
The caryotype study consists of the analysis of the woman's chromosomes. A simple blood test checks if the woman has a normal caryotype (46, XX) or if there is any chromosomal alteration that may be making it difficult to get pregnant. The alteration in the caryotype can be at the structural level or at the numerical level of the chromosomes.
It should be noted that caryotyping is a routine test performed in most cases of infertility, both in men and women. Moreover, this test is especially necessary when there are cases of repeated miscarriages or implantation failures.
Hysteroscopy (HSC)
Hysteroscopy is a medical procedure that allows the visualization of the interior of the uterine cavity thanks to the introduction of an endoscopic camera (hysteroscope). This is a simple and short outpatient procedure that allows the detection of polyps, fibroids and other malformations of the uterus that cannot be diagnosed with a simple ultrasound scan.
It should be noted that hysteroscopy does not allow the access into the fallopian tubes, but it is possible to observe the entrance holes to the tubes. The main reason why the hysteroscope cannot go through the fallopian tubes is because of the small diameter of the tubes.
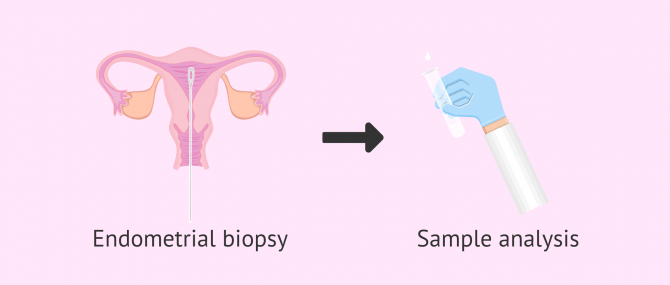
Endometrial biopsy
An endometrial biopsy is a diagnostic test that allows a small piece of the endometrium to be removed for analysis in the laboratory. Therefore, a biopsy catheter is inserted through the vagina and gently suctioned to remove a sample of the lining of the uterus.
In this way, any existing pathogen or abnormality in the uterus that could be preventing embryo implantation or the ascent of sperm in search of the egg can be studied.
The endometrial biopsy can be performed with or without local anesthesia in the office and the patient does not need any special preparation. If the test is not performed under anesthesia, the patient may feel discomfort, some pain, and/or cramping. In addition, endometrial biopsy is sometimes performed at the same time as hysteroscopy.
In assisted reproduction, like any medical treatment, it is necessary for you to trust the professionalism of the doctors and the clinic you choose.
This Tool generates you a personalized report with all information necessary about the treatment you will need. Besides, there is a list of clinics in your area which we have chosen based on our selection criteria with their budget plan included. Last but not least, you will find a series of useful tips for your first clinic visit.
FAQs from users
What are the main female infertility tests?
The main female infertility tests include:
- Blood test – Day FSH and E2, Anti mullerian hormone (AMH), TSH, Prolactin
- Tube test – Hysterosalpingogram
- Pelvic ultrasound with antral follicle count
How much does a female fertility test cost?
It depends on the tests required and the location where they are performed, but in general the cost of a basic female fertility study can range from $150 to $500 on average.
A hysterosalpingography can cost up to $800-3,000. As for a pelvic ultrasound, a pap smear, and a gynecological exam, the price can be $200 in total, and hormone blood tests can cost up to $50-200 each.
Are these tests painful?
The gynaecological examination is usually not painful, nor is the blood test. On the contrary, hysterosalpingography can cause discomfort or pain. There are women who simply notice a small discomfort of the same intensity as the cytology or any other gynaecological check-up, while there are other women who feel more pain.
How does a woman know if she is sterile?
First, the woman will need to go to a specialist to request a female fertility study.
If she is not trying to get pregnant, only a vaginal ultrasound and a pap smear are needed. These tests determine if the woman has any uterine abnormalities or any other pathology. In addition, a hormonal study is recommended to assess the woman's ovarian reserve.
If the woman has been having unprotected sexual relations regularly for a year and has not been able to get pregnant, a hysterosalpingography and a caryotype study should be carried out.
Suggested for you
If you are trying to get pregnant and are not successful, you may also be interested in information about male infertility studies. Therefore, we recommend you read the following article: How do I know if I'm sterile: male fertility tests.
If you want to know the main reasons that makes getting pregnant impossible, continue reading here: Sterility and inability to get pregnant: causes and possible solutions.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Authors and contributors







My doctor ordered me to undergo hysterosalpingography. What do I have to expect? Does it hurt or will it be carried out through sedation?
Hello Sheyla,
during a hysterosalpingography slight discomfort may appear in the abdomen but stops as soon as the doctor stops introducing the contrast fluid.
In any case, this is nothing to worry about and absolutely bearable without anesthesia.
Wish you all the best.
Is the blood test for karyotyping normal or does it require some additional pain or discomfort? In which cases is it done?
Hello Philipa,
the karyotype is tested from a normal blood sample. In other words, although this study is not included in the routine analysis, no special extraction is necessary and no specific instruments are required. The chromosomes are simply analysed from a blood sample taken by normal extraction, usually after a small puncture in the arm.
Karyotyping is usually indicated in cases of repeated miscarriages of unknown cause or cases of family history of chromosomal disease such as Down syndrome.
Hope this helps,
Best